
Treatment ct scan spine pdf free download - similar
Magnetic resonance imaging
Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes of the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from CT and PET scans. MRI is a medical application of nuclear magnetic resonance (NMR) which can also be used for imaging in other NMR applications, such as NMR spectroscopy.
While the hazards of ionizing radiation are now well controlled in most medical contexts[citation needed], an MRI may still be seen as a better choice than a CT scan. MRI is widely used in hospitals and clinics for medical diagnosis and staging and follow-up of disease without exposing the body to radiation. An MRI may yield different information compared with CT. Risks and discomfort may be associated with MRI scans. Compared with CT scans, MRI scans typically take longer and are louder, and they usually need the subject to enter a narrow, confining tube. In addition, people with some medical implants or other non-removable metal inside the body may be unable to undergo an MRI examination safely.
MRI was originally called NMRI (nuclear magnetic resonance imaging), but "nuclear" was dropped to avoid negative associations.[1] Certain atomic nuclei are able to absorb radio frequency energy when placed in an external magnetic field; the resultant evolving spin polarization can induce a RF signal in a radio frequency coil and thereby be detected.[2] In clinical and research MRI, hydrogen atoms are most often used to generate a macroscopic polarization that is detected by antennas close to the subject being examined.[2] Hydrogen atoms are naturally abundant in humans and other biological organisms, particularly in water and fat. For this reason, most MRI scans essentially map the location of water and fat in the body. Pulses of radio waves excite the nuclear spin energy transition, and magnetic field gradients localize the polarization in space. By varying the parameters of the pulse sequence, different contrasts may be generated between tissues based on the relaxation properties of the hydrogen atoms therein.
Since its development in the 1970s and 1980s, MRI has proven to be a versatile imaging technique. While MRI is most prominently used in diagnostic medicine and biomedical research, it also may be used to form images of non-living objects. MRI scans are capable of producing a variety of chemical and physical data, in addition to detailed spatial images. The sustained increase in demand for MRI within health systems has led to concerns about cost effectiveness and overdiagnosis.[3][4]
Mechanism[edit]
Construction and physics[edit]

In most medical applications, hydrogen nuclei, which consist solely of a proton, that are in tissues create a signal that is processed to form an image of the body in terms of the density of those nuclei in a specific region. Given that the protons are affected by fields from other atoms to which they are bonded, it is possible to separate responses from hydrogen in specific compounds. To perform a study, the person is positioned within an MRI scanner that forms a strong magnetic field around the area to be imaged. First, energy from an oscillating magnetic field is temporarily applied to the patient at the appropriate resonance frequency. Scanning with X and Y gradient coils cause a selected region of the patient to experience the exact magnetic field required for the energy to be absorbed. The excited atoms emit a radio frequency (RF) signal, which is measured by a receiving coil. The RF signal may be processed to deduce position information by looking at the changes in RF level and phase caused by varying the local magnetic field using gradient coils. As these coils are rapidly switched during the excitation and response to perform a moving line scan, they create the characteristic repetitive noise of an MRI scan as the windings move slightly due to magnetostriction. The contrast between different tissues is determined by the rate at which excited atoms return to the equilibrium state. Exogenouscontrast agents may be given to the person to make the image clearer.[5]
The major components of an MRI scanner are the main magnet, which polarizes the sample, the shim coils for correcting shifts in the homogeneity of the main magnetic field, the gradient system which is used to localize the region to be scanned and the RF system, which excites the sample and detects the resulting NMR signal. The whole system is controlled by one or more computers.

 | A short extract of a 20-minute scanning session, recorded outside the above unit |
Problems playing this file? See media help. | |
MRI requires a magnetic field that is both strong and uniform to a few parts per million across the scan volume. The field strength of the magnet is measured in teslas – and while the majority of systems operate at 1.5 T, commercial systems are available between 0.2 and 7 T. Most clinical magnets are superconducting magnets, which require liquid helium to keep them very cold. Lower field strengths can be achieved with permanent magnets, which are often used in "open" MRI scanners for claustrophobic patients.[6] Lower field strengths are also used in a portable MRI scanner approved by the FDA in 2020.[7] Recently, MRI has been demonstrated also at ultra-low fields, i.e., in the microtesla-to-millitesla range, where sufficient signal quality is made possible by prepolarization (on the order of 10–100 mT) and by measuring the Larmor precession fields at about 100 microtesla with highly sensitive superconducting quantum interference devices (SQUIDs).[8][9][10]
T1 and T2[edit]
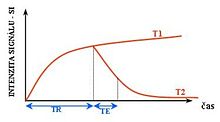

Each tissue returns to its equilibrium state after excitation by the independent relaxation processes of T1 (spin-lattice; that is, magnetization in the same direction as the static magnetic field) and T2 (spin-spin; transverse to the static magnetic field). To create a T1-weighted image, magnetization is allowed to recover before measuring the MR signal by changing the repetition time (TR). This image weighting is useful for assessing the cerebral cortex, identifying fatty tissue, characterizing focal liver lesions, and in general, obtaining morphological information, as well as for post-contrast imaging. To create a T2-weighted image, magnetization is allowed to decay before measuring the MR signal by changing the echo time (TE). This image weighting is useful for detecting edema and inflammation, revealing white matter lesions, and assessing zonal anatomy in the prostate and uterus.
The standard display of MRI images is to represent fluid characteristics in black and white images, where different tissues turn out as follows:
| Signal | T1-weighted | T2-weighted |
|---|---|---|
| High | ||
| Inter- mediate | Gray matter darker than white matter[13] | White matter darker than grey matter[13] |
| Low |
Diagnostics[edit]
Usage by organ or system[edit]

MRI has a wide range of applications in medical diagnosis and more than 25,000 scanners are estimated to be in use worldwide.[14] MRI affects diagnosis and treatment in many specialties although the effect on improved health outcomes is disputed in certain cases.[15][16]
MRI is the investigation of choice in the preoperative staging of rectal and prostate cancer and has a role in the diagnosis, staging, and follow-up of other tumors,[17] as well as for determining areas of tissue for sampling in biobanking.[18][19]
Neuroimaging[edit]
MRI is the investigative tool of choice for neurological cancers over CT, as it offers better visualization of the posterior cranial fossa, containing the brainstem and the cerebellum. The contrast provided between grey and white matter makes MRI the best choice for many conditions of the central nervous system, including demyelinating diseases, dementia, cerebrovascular disease, infectious diseases, Alzheimer's disease and epilepsy.[20][21][22] Since many images are taken milliseconds apart, it shows how the brain responds to different stimuli, enabling researchers to study both the functional and structural brain abnormalities in psychological disorders.[23] MRI also is used in guidedstereotactic surgery and radiosurgery for treatment of intracranial tumors, arteriovenous malformations, and other surgically treatable conditions using a device known as the N-localizer.[24][25][26]
Cardiovascular[edit]

Cardiac MRI is complementary to other imaging techniques, such as echocardiography, cardiac CT, and nuclear medicine. It can be used to assess the structure and the function of the heart.[27] Its applications include assessment of myocardial ischemia and viability, cardiomyopathies, myocarditis, iron overload, vascular diseases, and congenital heart disease.[28]
Musculoskeletal[edit]
Applications in the musculoskeletal system include spinal imaging, assessment of joint disease, and soft tissue tumors.[29] Also, MRI techniques can be used for diagnostic imaging of systemic muscle diseases.[30]
Liver and gastrointestinal[edit]
Hepatobiliary MR is used to detect and characterize lesions of the liver, pancreas, and bile ducts. Focal or diffuse disorders of the liver may be evaluated using diffusion-weighted, opposed-phase imaging and dynamic contrast enhancement sequences. Extracellular contrast agents are used widely in liver MRI, and newer hepatobiliary contrast agents also provide the opportunity to perform functional biliary imaging. Anatomical imaging of the bile ducts is achieved by using a heavily T2-weighted sequence in magnetic resonance cholangiopancreatography (MRCP). Functional imaging of the pancreas is performed following administration of secretin. MR enterography provides non-invasive assessment of inflammatory bowel disease and small bowel tumors. MR-colonography may play a role in the detection of large polyps in patients at increased risk of colorectal cancer.[31][32][33][34]
Angiography[edit]
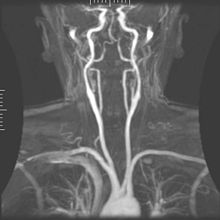
Magnetic resonance angiography (MRA) generates pictures of the arteries to evaluate them for stenosis (abnormal narrowing) or aneurysms (vessel wall dilatations, at risk of rupture). MRA is often used to evaluate the arteries of the neck and brain, the thoracic and abdominal aorta, the renal arteries, and the legs (called a "run-off"). A variety of techniques can be used to generate the pictures, such as administration of a paramagnetic contrast agent (gadolinium) or using a technique known as "flow-related enhancement" (e.g., 2D and 3D time-of-flight sequences), where most of the signal on an image is due to blood that recently moved into that plane (see also FLASH MRI).[35]
Techniques involving phase accumulation (known as phase contrast angiography) can also be used to generate flow velocity maps easily and accurately. Magnetic resonance venography (MRV) is a similar procedure that is used to image veins. In this method, the tissue is now excited inferiorly, while the signal is gathered in the plane immediately superior to the excitation plane—thus imaging the venous blood that recently moved from the excited plane.[36]
Contrast agents[edit]
MRI for imaging anatomical structures or blood flow do not require contrast agents since the varying properties of the tissues or blood provide natural contrasts. However, for more specific types of imaging, exogenous contrast agents may be given intravenously, orally, or intra-articularly.[5] The most commonly used intravenous contrast agents are based on chelates of gadolinium.[37] In general, these agents have proved safer than the iodinated contrast agents used in X-ray radiography or CT. Anaphylactoid reactions are rare, occurring in approx. 0.03–0.1%.[38] Of particular interest is the lower incidence of nephrotoxicity, compared with iodinated agents, when given at usual doses—this has made contrast-enhanced MRI scanning an option for patients with renal impairment, who would otherwise not be able to undergo contrast-enhanced CT.[39]
In December 2017, the Food and Drug Administration (FDA) in the United States announced in a drug safety communication that new warnings were to be included on all gadolinium-based contrast agents (GBCAs). The FDA also called for increased patient education and requiring gadolinium contrast vendors to conduct additional animal and clinical studies to assess the safety of these agents.[40] Although gadolinium agents have proved useful for patients with kidney impairment, in patients with severe kidney failure requiring dialysis there is a risk of a rare but serious illness, nephrogenic systemic fibrosis, which may be linked to the use of certain gadolinium-containing agents. The most frequently linked is gadodiamide, but other agents have been linked too.[41] Although a causal link has not been definitively established, current guidelines in the United States are that dialysis patients should only receive gadolinium agents where essential and that dialysis should be performed as soon as possible after the scan to remove the agent from the body promptly.[42][43]
In Europe, where more gadolinium-containing agents are available, a classification of agents according to potential risks has been released.[44][45] In 2008, a new contrast agent named gadoxetate, brand name Eovist (US) or Primovist (EU), was approved for diagnostic use: This has the theoretical benefit of a dual excretion path.[46]
Sequences[edit]
An MRI sequence is a particular setting of radiofrequency pulses and gradients, resulting in a particular image appearance.[47] The T1 and T2 weighting can also be described as MRI sequences.
Overview table
edit
This table does not include uncommon and experimental sequences.
| Group | Sequence | Abbr. | Physics | Main clinical distinctions | Example |
|---|---|---|---|---|---|
| Spin echo | T1 weighted | T1 | Measuring spin–lattice relaxation by using a short repetition time (TR) and echo time (TE). | Standard foundation and comparison for other sequences |  |
| T2 weighted | T2 | Measuring spin–spin relaxation by using long TR and TE times | Standard foundation and comparison for other sequences |  | |
| Proton density weighted | PD | Long TR (to reduce T1) and short TE (to minimize T2).[50] | Joint disease and injury.[51] |  | |
| Gradient echo (GRE) | Steady-state free precession | SSFP | Maintenance of a steady, residual transverse magnetisation over successive cycles.[53] | Creation of cardiac MRI videos (pictured).[53] |  |
| Effective T2 or "T2-star" | T2* | Postexcitation refocused GRE with small flip angle.[54] | Low signal from hemosiderin deposits (pictured) and hemorrhages.[54] |  | |
| Inversion recovery | Short tau inversion recovery | STIR | Fat suppression by setting an inversion time where the signal of fat is zero.[55] | High signal in edema, such as in more severe stress fracture.[56]Shin splints pictured: |  |
| Fluid-attenuated inversion recovery | FLAIR | Fluid suppression by setting an inversion time that nulls fluids | High signal in lacunar infarction, multiple sclerosis (MS) plaques, subarachnoid haemorrhage and meningitis (pictured).[57] |  | |
| Double inversion recovery | DIR | Simultaneous suppression of cerebrospinal fluid and white matter by two inversion times.[58] | High signal of multiple sclerosis plaques (pictured).[58] |  | |
| Diffusion weighted (DWI) | Conventional | DWI | Measure of Brownian motion of water molecules.[59] | High signal within minutes of cerebral infarction (pictured).[60] |  |
| Apparent diffusion coefficient | ADC | Reduced T2 weighting by taking multiple conventional DWI images with different DWI weighting, and the change corresponds to diffusion.[61] | Low signal minutes after cerebral infarction (pictured).[62] |  | |
| Diffusion tensor | DTI | Mainly tractography (pictured) by an overall greater Brownian motion of water molecules in the directions of nerve fibers.[63] |  | ||
| Perfusion weighted (PWI) | Dynamic susceptibility contrast | DSC | Gadolinium contrast is injected, and rapid repeated imaging (generally gradient-echo echo-planar T2 weighted) quantifies susceptibility-induced signal loss.[65] | In cerebral infarction, the infarcted core and the penumbra have decreased perfusion (pictured).[66] |  |
| Dynamic contrast enhanced | DCE | Measuring shortening of the spin–lattice relaxation (T1) induced by a gadolinium contrast bolus.[67] | |||
| Arterial spin labelling | ASL | Magnetic labeling of arterial blood below the imaging slab, which subsequently enters the region of interest.[68] It does not need gadolinium contrast.[69] | |||
| Functional MRI (fMRI) | Blood-oxygen-level dependent imaging | BOLD | Changes in oxygen saturation-dependent magnetism of hemoglobin reflects tissue activity.[70] | Localizing highly active brain areas before surgery, also used in research of cognition.[71] |  |
| Magnetic resonance angiography (MRA) and venography | Time-of-flight | TOF | Blood entering the imaged area is not yet magnetically saturated, giving it a much higher signal when using short echo time and flow compensation. | Detection of aneurysm, stenosis, or dissection[72] |  |
| Phase-contrast magnetic resonance imaging | PC-MRA | Two gradients with equal magnitude, but opposite direction, are used to encode a phase shift, which is proportional to the velocity of spins.[73] | Detection of aneurysm, stenosis, or dissection (pictured).[72] |  (VIPR) | |
| Susceptibility-weighted | SWI | Sensitive for blood and calcium, by a fully flow compensated, long echo, gradient recalled echo (GRE) pulse sequence to exploit magnetic susceptibility differences between tissues | Detecting small amounts of hemorrhage (diffuse axonal injury pictured) or calcium.[74] |  | |
Other specialized configurations[edit]
Magnetic resonance spectroscopy[edit]
Magnetic resonance spectroscopy (MRS) is used to measure the levels of different metabolites in body tissues, which can be achieved through a variety of single voxel or imaging-based techniques.[75] The MR signal produces a spectrum of resonances that corresponds to different molecular arrangements of the isotope being "excited". This signature is used to diagnose certain metabolic disorders, especially those affecting the brain,[76] and to provide information on tumor metabolism.[77]
Magnetic resonance spectroscopic imaging (MRSI) combines both spectroscopic and imaging methods to produce spatially localized spectra from within the sample or patient. The spatial resolution is much lower (limited by the available SNR), but the spectra in each voxel contains information about many metabolites. Because the available signal is used to encode spatial and spectral information, MRSI requires high SNR achievable only at higher field strengths (3 T and above).[78] The high procurement and maintenance costs of MRI with extremely high field strengths[79] inhibit their popularity. However, recent compressed sensing-based software algorithms (e.g., SAMV[80]) have been proposed to achieve super-resolution without requiring such high field strengths.
Real-time MRI[edit]
Real-time MRI refers to the continuous imaging of moving objects (such as the heart) in real time. One of the many different strategies developed since the early 2000s is based on radial FLASH MRI, and iterative reconstruction. This gives a temporal resolution of 20–30 ms for images with an in-plane resolution of 1.5–2.0 mm.[81] Balanced steady-state free precession (bSSFP) imaging has a better image contrast between the blood pool and myocardium than the FLASH MRI, yet it will produce severe banding artifact when the B0 inhomogeneity is strong. Real-time MRI is likely to add important information on diseases of the heart and the joints, and in many cases may make MRI examinations easier and more comfortable for patients, especially for the patients who cannot hold their breathings or who have arrhythmia.[82]
Interventional MRI[edit]
The lack of harmful effects on the patient and the operator make MRI well-suited for interventional radiology, where the images produced by an MRI scanner guide minimally invasive procedures. Such procedures use no ferromagnetic instruments.[83]
A specialized growing subset of interventional MRI is intraoperative MRI, in which an MRI is used in surgery. Some specialized MRI systems allow imaging concurrent with the surgical procedure. More typically, the surgical procedure is temporarily interrupted so that MRI can assess the success of the procedure or guide subsequent surgical work.[84]
Magnetic resonance guided focused ultrasound[edit]
In guided therapy, high-intensity focused ultrasound (HIFU) beams are focused on a tissue, that are controlled using MR thermal imaging. Due to the high energy at the focus, the temperature rises to above 65 °C (150 °F) which completely destroys the tissue. This technology can achieve precise ablation of diseased tissue. MR imaging provides a three-dimensional view of the target tissue, allowing for the precise focusing of ultrasound energy. The MR imaging provides quantitative, real-time, thermal images of the treated area. This allows the physician to ensure that the temperature generated during each cycle of ultrasound energy is sufficient to cause thermal ablation within the desired tissue and if not, to adapt the parameters to ensure effective treatment.[85]
Multinuclear imaging[edit]
Hydrogen has the most frequently imaged nucleus in MRI because it is present in biological tissues in great abundance, and because its high gyromagnetic ratio gives a strong signal. However, any nucleus with a net nuclear spin could potentially be imaged with MRI. Such nuclei include helium-3, lithium-7, carbon-13, fluorine-19, oxygen-17, sodium-23, phosphorus-31 and xenon-129. 23Na and 31P are naturally abundant in the body, so they can be imaged directly. Gaseous isotopes such as 3He or 129Xe must be hyperpolarized and then inhaled as their nuclear density is too low to yield a useful signal under normal conditions. 17O and 19F can be administered in sufficient quantities in liquid form (e.g. 17O-water) that hyperpolarization is not a necessity.[86]
Treatment ct scan spine pdf free download - interesting


-
-
-